What is Prior Authorization?
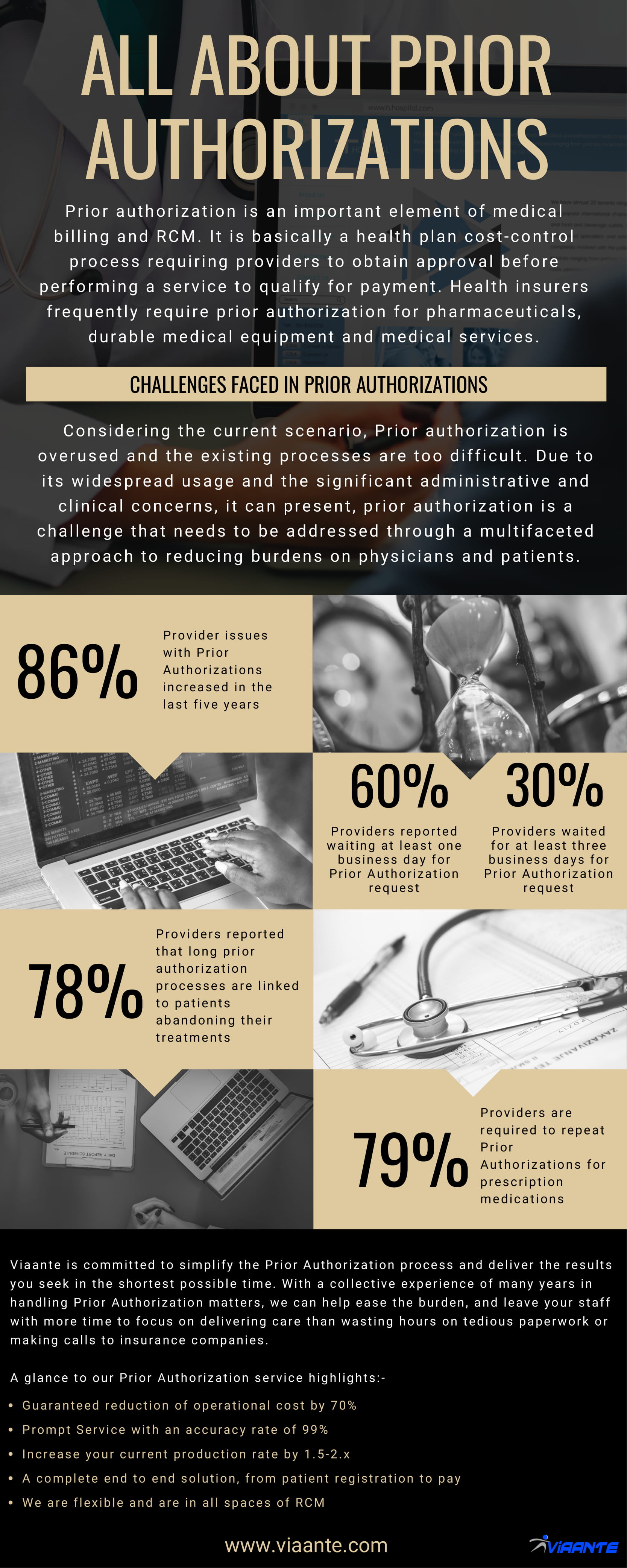
Prior authorization is an important element of medical billing and RCM. It is basically a health plan cost-control process requiring providers to obtain approval before performing a service to qualify for payment. Health insurers frequently require prior authorization for pharmaceuticals, durable medical equipment and medical services.
It is one of the most exhausting and difficult components in the entire revenue cycle. It can interrupt workflow,
Considering the current scenario

Challenges in Prior Authorizations:-
The inefficiency and lack of transparency associated with prior authorization cost physician practices time and money. The lengthy processes may also have negative consequences for patient outcomes when treatment is delayed.
In the current managed care environment, an increasing number of prescriptions are being denied by plans, requiring prescribers to complete prior authorizations. This process is highly disruptive,
Plans are making PA forms more complex and are changing them frequently. When a call to a plan is required, it is common for a prescriber or their staff to spend several minutes on hold before ever speaking with anyone at the plan. Nurses, practice managers, or other staffs who are charged with completing and submitting PA forms find the process to be confusing, time-consuming, and frustrating.
Here are some key challenges faced in Prior Authorization:-
- Prior authorization issues are associated with 92 percent of care delays and may also contribute to patient safety concerns as well as administrative inefficiencies
- Prior authorization process can be a lengthy administrative nightmare of recurring paperwork, multiple phone calls and bureaucratic battles that can delay or disrupt a patient’s access to vital care
- 64%of providers reported waiting for at least one business day for a prior authorization request and 30% waited for at least three business days
- 78%of providers reported that long prior authorization processes are linked to patients abandoning their treatments
- Providers take 14.6 hours on an average to complete these requests, which is the equivalent of two business days. 34% percent of providers have staff dedicated exclusively to complete prior authorizations
Time spent in a week by various Personnel of Prior Authorization

5% of time Primary Care Physician

30% of time Nursing Staff

12% of time Clerical Staff
Services requiring Prior Authorization:-
- Therapy (speech, occupational, and physical)
- Plastic Surgery
- Durable Medical Equipment (DME)
- Inpatient
- Home-Based Services
- Pharmacy and Medications
- Pain Management
- Advanced Outpatient Imaging Services
- Services Requiring Notifications (All newborn deliveries-Maternity obstetrical services, outpatient care, etc.)
Here are some tips you and your practice can take to minimize the costs and time required to obtain prior authorization from a payer for a medication or procedure:
- Whenever possible, use the payer’s web site rather than the telephone
- Look at how many prior authorizations each of your payers required during the past year, and consider dropping them if the payer’s reimbursement rates don’t justify your time spent obtaining the authorizations.
- If you’re in a multi-site practice, designate one or two individuals to handle prior authorization for the entire practice. Make sure those individuals have access to patients’ records and providers’ notes from throughout the practice.
- Make sure you are following recommended treatment guidelines before ordering a high-cost procedure for a patient.
- Unless contraindicated, always start patients on the generic form of medication if one is available in the same therapeutic class.
- Make sure you’ve met all of the payer’s criteria before submitting prior authorization requests.
Viaante is a HIPAA compliant Healthcare Service Provider offering quality and customized services, which helps the healthcare firms in improving business process efficiencies, deliver superior customer service experience and boost their financial performance. Viaante has years of experience and expertise in delivering accurate, high quality, cost-efficient and streamlined BPO services that boost up the performance of the organization. Viaante is committed to simplify the Prior Authorization process and deliver the results you seek in the shortest possible time. For assistance in services related to Prior Authorizations and more, visit our website www.viaante.com or reach us at marketing@viaante.com
FAQ’s
How does outsourcing PriorAuth keep my information safe?
Viaante is a HIPAA and PHI compliant Healthcare Service Provider offering quality and customized services, which helps the healthcare firms in improving business process efficiencies, deliver superior customer service experience with high level of security.
How does your prior authorizations services work?
Our prior auths team comes with a rich experience working with various payor mix. Our resources call up the payers manually to get the approval in a short span of time. We maintain an acciracy level of over 99% with a STAT turnaround time of 15-20 minutes.
Why outsource Prior Authorizations services to Viaante?
Viaante is committed to simplify the Prior Authorization process and deliver the results you seek in the shortest possible time. Outsource Prior Authorization services to Viaante in order to achieve:-
- Guaranteed reduction of operational cost by 70%
- Prompt Service with a accuracy rate of 99%
- Durable Medical Equipment (DME)
- Increase your current production rate by 1.5-2.x
- We are flexible and are in all spaces of RCM