17th October 2025
Estimated reading time : 7 Minutes
Master Risk Adjustment Coding in Healthcare: The Key to Boost Revenue and Compliance
What is Risk Adjustment Coding and why it’s Crucial
In the complex landscape of modern healthcare finance, particularly in value-based payment models like Medicare Advantage, precise and complete documentation is paramount. At the heart of this system lies Risk Adjustment Coding.
What is risk adjustment coding? It’s a methodology used by payers (like Medicare, Medicaid, and commercial plans) to estimate the expected healthcare costs for a patient population. This is achieved by assigning a Risk Adjustment Factor (RAF) score to each patient. The RAF score is a numerical reflection of a patient’s predicted healthcare costs for the year, factoring in their demographic details and chronic conditions.
The primary function is to ensure financial fairness. A health plan covering patients with numerous severe chronic conditions (a high-risk population) will naturally incur higher costs than a plan with a healthier population. Risk adjustment compensates these plans appropriately, providing them with the necessary funds to manage the full burden of illness for their enrollees.
The Direct Link to Revenue
For providers, accurate risk adjustment coding is not merely a compliance task—it’s a direct lever for revenue optimization and sustainability.
- Fair Reimbursement: Correctly documenting and coding all chronic conditions ensures providers are adequately reimbursed for the complexity and severity of the patients they manage. Under-coding, or failing to capture all relevant conditions, leads to an inaccurate, lower RAF score and, consequently, underpayment.
- Funding Quality Care: Higher, accurate reimbursement allows health systems to invest in the resources, staff, and programs needed to provide high-quality care, especially for complex, chronically ill patients.
Risk Adjustment Documentation and Coding Essentials: The MEAT Principle
The cornerstone of successful risk adjustment coding is comprehensive and specific clinical documentation. Coders rely entirely on the provider’s medical record to assign the correct diagnosis codes (ICD-10-CM), which then map to Hierarchical Condition Categories (HCCs) used to calculate the RAF score.
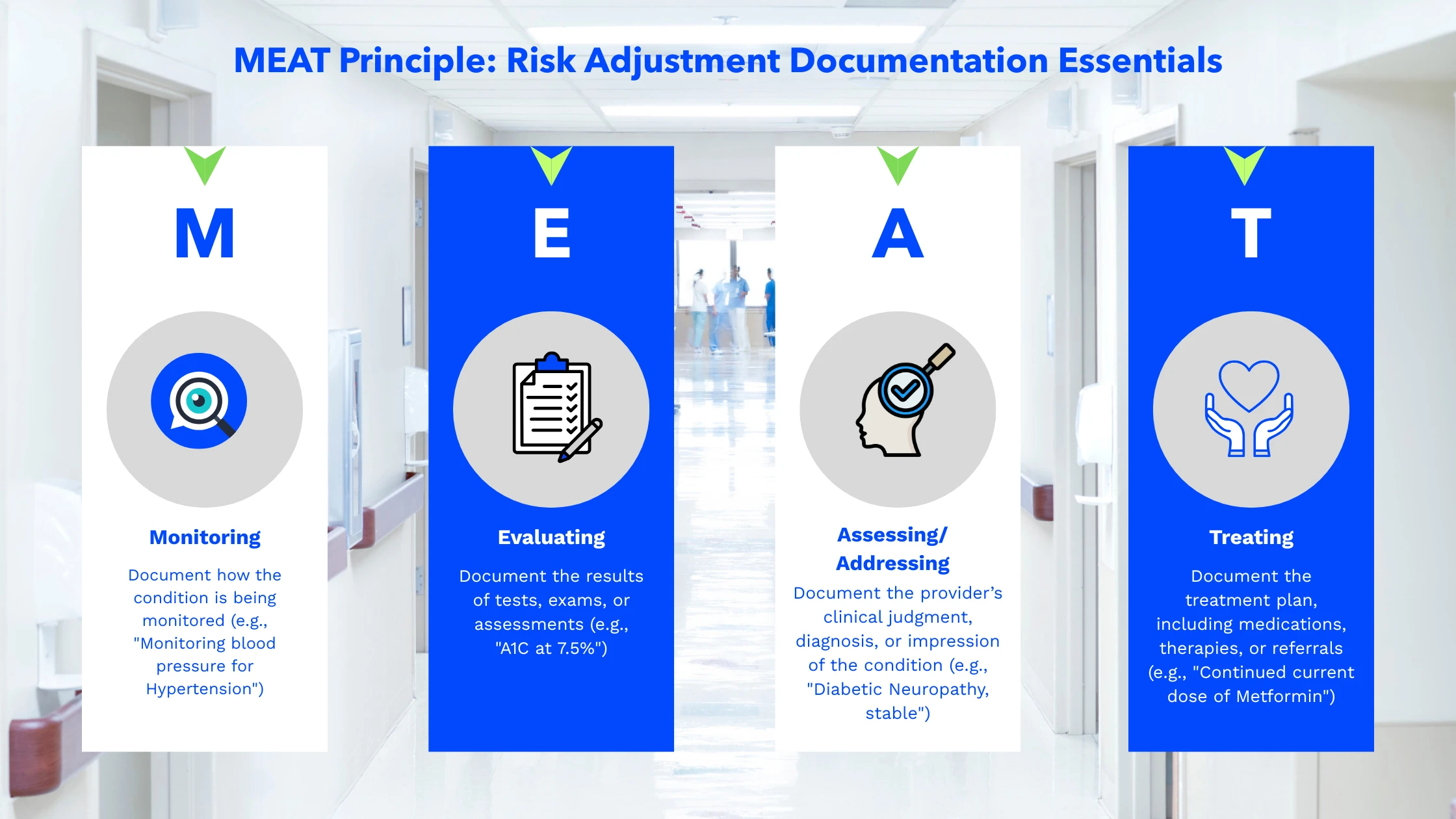
To ensure your documentation meets the required standards, adopt the MEAT principle for every chronic condition addressed during a patient encounter (Below is an image that visually represents the MEAT acronym and its components)
Crucial Coding Rule: All chronic conditions must be documented and submitted on a claim at least once per calendar year to be included in the annual RAF calculation. If a chronic condition is present and affects patient care, it must be captured with the highest level of specificity.
Provider Education is Key to Improving Risk Adjustment Coding Compliance
The most significant barrier to accurate risk adjustment is often a lack of understanding or focus at the point of care. Providers—physicians, physician assistants, and nurse practitioners—are the primary source of the documentation that drives the entire process. Effective, ongoing education is non-negotiable for improving compliance and revenue.
Core Education Focus Areas:
- The ‘Why’ of Specificity: Training must go beyond listing rules. Providers need to understand why “Type 2 Diabetes with moderate No proliferative Diabetic Retinopathy” (specific) codes and reimburses differently than simply “Diabetes” (non-specific).
- MEAT Documentation: Consistent training on the MEAT principle ensures providers include the necessary clinical support for every diagnosis they list. Documentation must clearly show the condition is active, current, and managed.
- Annual Refresh: Because the RAF score resets every January 1st, providers must be reminded to document and “re-establish” all active chronic conditions for every patient at least once in the new calendar year.
- Audit Preparedness: Educating providers on the importance of legibility, timely signatures, and the compliance risks of unsupported documentation (which can lead to costly audits and recoupments) reinforces the financial and legal urgency of accurate coding.
Ways to Improve Risk Adjustment Coding Compliance and Capture
Achieving and maintaining high risk adjustment coding compliance is an organizational effort, requiring strategic integration of people, processes, and technology.
Integrate Coding into Clinical Workflow
- EHR Optimization: Utilize your Electronic Health Record (EHR) system to prompt providers. Tools like dynamic problem lists that flag unaddressed chronic conditions or clinical decision support that suggests high-specificity codes at the point-of-care can significantly improve accuracy.
- Annual Wellness Visits (AWVs): Strategically use the AWV as a dedicated opportunity to perform a comprehensive annual review of all chronic conditions and update the patient’s entire health profile, ensuring all active HCCs are captured early in the year.
Implement Targeted Chart Reviews
- Retrospective Review: Conduct reviews of submitted claims and medical records to identify diagnoses that were documented but not coded, or conditions that were coded inaccurately. This helps recover lost revenue and informs future provider education.
- Prospective Review: Use data analytics to identify patients with a strong likelihood of having an uncaptured HCC (e.g., a patient on a high-risk medication but with no corresponding diagnosis code). This allows coders to alert providers to documentation gaps before the patient’s visit, enabling proactive capture.
Establish a Clinical Documentation Integrity (CDI) Program
A specialized CDI team, which includes coders and clinical staff, can work collaboratively with providers. Their role is to:
- Query Providers: Submit specific, non-leading queries to providers when documentation is unclear, non-specific, or lacks the necessary MEAT support.
- Develop Internal Guidelines: Create clear, organization-specific documentation guidelines for common complex conditions (e.g., Chronic Kidney Disease staging, documentation for Morbid Obesity) to ensure consistency.
Conclusion: Securing Your Revenue Cycle with Accurate Risk Adjustment
In a healthcare environment increasingly driven by value-based care, accurate risk adjustment coding is no longer optional—it’s foundational. By committing to continuous provider education, robust documentation practices, and strategic integration of coding workflows, your organization can ensure its Risk Adjustment Factor (RAF) scores accurately reflect the true complexity of your patient population. This commitment to compliance is the surest path to boosting revenue and securing financial stability for the long term.
Need expert support to navigate the complexities of risk adjustment and optimize your financial health?
Viaante Business Solution provides comprehensive Revenue Cycle Management (RCM) solutions, including specialized expertise in risk adjustment coding, clinical documentation improvement, and end-to-end claim management. Partner with us to ensure maximum compliance, accurate reimbursement, and sustained financial success.







