14th January 2026
Estimated reading time : 7 Minutes
Medical Billing vs Medical Coding: Understanding the Key Differences That Impact Revenue Cycle Success
Healthcare organizations often struggle to distinguish between medical billing and medical coding, yet these functions serve distinct purposes in revenue cycle management. While both are essential to capturing reimbursement, confusing their roles can lead to claim denials, compliance issues, and revenue leakage.
Understanding the difference between medical billing and medical coding matters because each function directly impacts cash flow, regulatory compliance, and audit outcomes. Providers, payers, and revenue cycle leaders need clarity on how these processes work individually and together to maintain financial health.
What Is Medical Coding?
Medical coding translates clinical documentation into standardized alphanumeric codes that represent diagnoses, procedures, services, and medical equipment. Coders review physician notes, lab results, and medical records to assign codes that insurance companies and government payers recognize.
Real-world example: When a patient visits for diabetes management, the coder assigns ICD-10-CM code E11.9 (Type 2 diabetes without complications) and CPT code 99214 (established patient office visit, moderate complexity).
Types of Medical Codes
ICD-10-CM – Diagnosis codes identifying patient conditions, symptoms, and diseases. The U.S. uses over 70,000 ICD-10-CM codes.
CPT – Procedure codes maintained by the American Medical Association describing medical services, surgeries, evaluations, and treatments.
HCPCS Level II – Codes for medical supplies, durable medical equipment, ambulance services, and procedures not covered by CPT.
Role and Impact
What Is Medical Billing?
Medical billing manages the end-to-end process of submitting claims to insurance companies and following through until payment is received. Billers transform coded clinical information into insurance claims, track their progress, and resolve issues that prevent reimbursement.
Key Steps in Medical Billing
Charge Entry – Billers enter procedure codes, diagnosis codes, and charges into the billing system, linking services to patient accounts and insurance information.
Claim Submission – Claims are electronically transmitted to insurance companies through clearinghouses that validate data before forwarding to payers.
Payer Follow-ups – Billers track claim status, respond to payer requests, and investigate payment delays.
Denial Management – Billers analyze denial reasons, correct errors, gather documentation, and resubmit or appeal denied claims.
Payment Posting – Billers record payments, reconcile explanation of benefits, and identify underpayments or overpayments.
Role and Impact on Cash Flow
Medical Coding vs Medical Billing: Key Differences
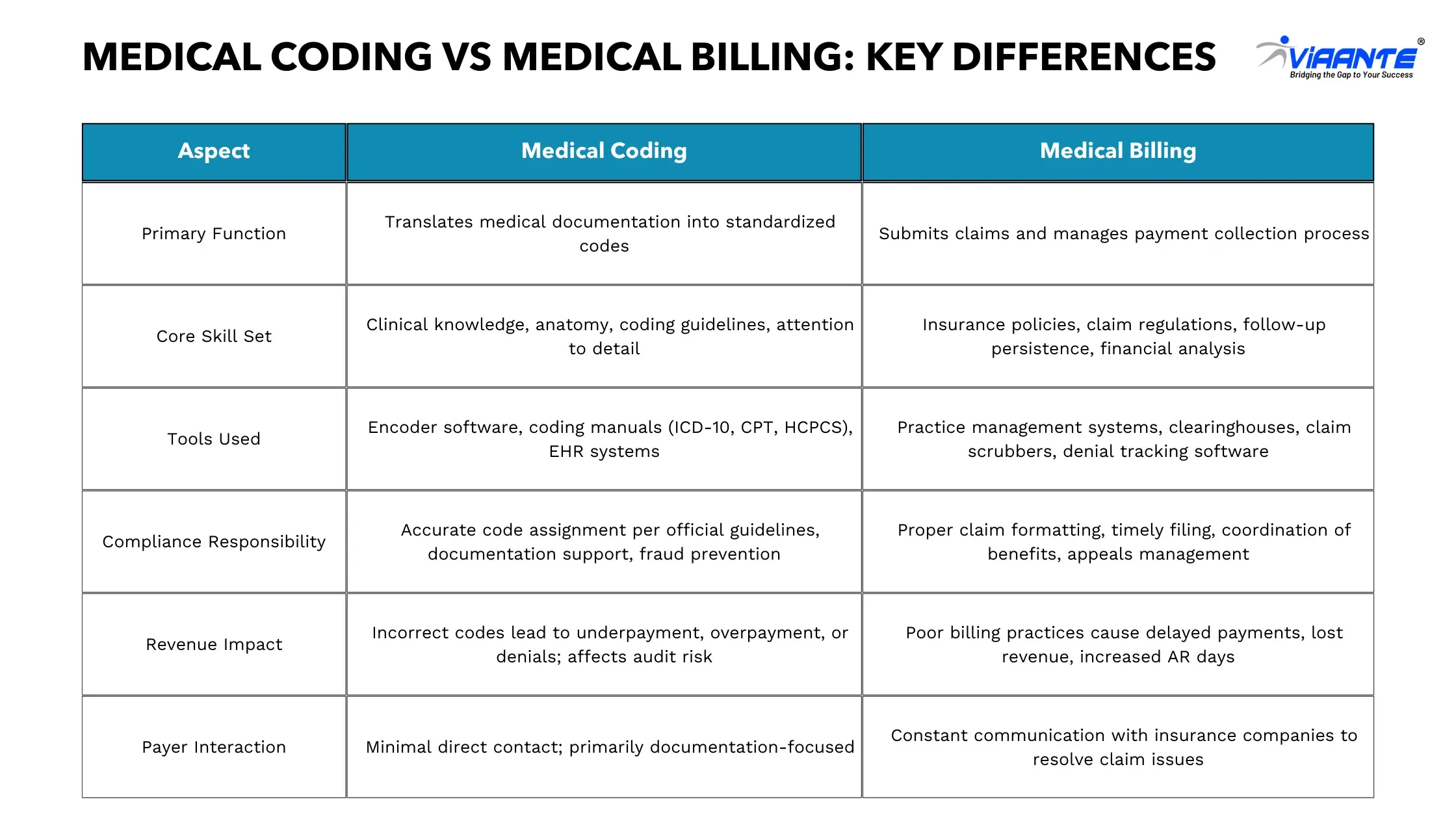
Medical Biller vs Medical Coder: Roles and Responsibilities
Day-to-Day Tasks
Medical Coders: Review physician documentation, research appropriate diagnosis and procedure codes, ensure documentation supports medical necessity, query providers for clarification, maintain knowledge of coding updates, and audit coded claims for accuracy.
Medical Billers: Verify patient insurance eligibility, enter charges and submit claims, monitor claim status, investigate and appeal denials, post payments and adjust accounts, generate patient statements, and track performance metrics like clean claim rate and AR days.
Skills Required
Coding Skills: Strong analytical abilities to interpret clinical documentation and apply complex coding rules. Coders need medical terminology, anatomy, physiology knowledge, critical thinking, and attention to detail—a single incorrect digit can change a code’s meaning entirely.
Billing Skills: Knowledge of insurance policies, claim submission requirements, and payer-specific rules. Billers need communication skills to resolve claim issues, problem-solving abilities to identify denial reasons, and persistence for following up on unpaid claims.
Certifications
Coding: CPC (Certified Professional Coder) – AAPC, CCS (Certified Coding Specialist) – AHIMA, COC (Certified Outpatient Coder) – AAPC, CIC (Certified Inpatient Coder) – AAPC
Billing: CPB (Certified Professional Biller) – AAPC, CMRS (Certified Medical Reimbursement Specialist) – AMBA, CBCS (Certified Billing and Coding Specialist) – NHA
Many healthcare employers prefer or require certification, particularly for remote positions.
Common Errors
Coding: Upcoding, downcoding, unbundling, missing or incorrect modifiers, lack of medical necessity documentation, incorrect diagnosis code sequencing
Billing: Typographical errors in patient demographics, submitting claims to incorrect insurers, missing prior authorizations, failing to check eligibility, delayed follow-ups, incorrect payment posting
Which Is Easier: Medical Billing or Medical Coding?
Neither role is objectively easier—they differ in complexity and pressure points based on individual strengths and interests.
Skill Complexity and Learning Curve
Medical coding requires deeper clinical knowledge of medical terminology, anatomy, surgical procedures, and disease processes. Coders work with tens of thousands of possible codes and detailed coding guidelines. Training programs take 12-18 months, with proficiency requiring 1-2 years of practical experience.
Medical billing demands comprehensive knowledge of insurance regulations and payer-specific requirements. Billers navigate complex insurance policies, coordination of benefits, and denial resolution strategies. Training programs are shorter (6-12 months), and new billers become productive more quickly, though mastering denial management takes time.
Risk and Compliance Pressure
Coding errors carry significant compliance risk under the False Claims Act, triggering audits, recoupment demands, and potential legal action. CMS, the Office of Inspector General, and Recovery Audit Contractors regularly audit coding practices.
Billing errors typically result in claim denials or delayed payments rather than compliance violations. While billing mistakes impact cash flow, they carry less regulatory risk than coding errors.
Career Paths
Coding: Medical Coder → Senior Coder → Coding Specialist → Coding Auditor → Coding Manager → Director of Health Information Management
Billing: Medical Biller → Senior Biller → Billing Specialist → Denial Manager → Revenue Cycle Analyst → Revenue Cycle Manager → Director of Revenue Cycle Operations
Both careers offer strong advancement opportunities, with advanced certifications and specialization increasing earning potential in both fields.
How Medical Billing and Coding Work Together
Medical billing and coding function as an integrated workflow where each role depends on the other for revenue cycle success.
Workflow Integration
The typical workflow sequence:
- Patient receives medical services from provider
- Provider documents the encounter in the medical record
- Medical coder reviews documentation and assigns appropriate codes
- Coded information transfers to billing system
- Medical biller validates patient insurance and submits claim electronically
- Payer adjudicates claim and issues payment or denial
- Biller posts payments or works denials back to resolution
Seamless communication between coders and billers is essential. When documentation is unclear, billers identify issues during claim scrubbing and alert coders. When claims are denied for coding reasons, billers work with coders to correct errors.
Impact of Coding Errors
Coding errors create immediate problems. When a coder assigns an incorrect code or fails to establish medical necessity, the claim is denied. This rework extends the revenue cycle by 30-60 days or more, increasing administrative costs and delaying cash flow. Studies show 50% of insurance denials result from billing and coding mistakes.
When billing and coding don’t collaborate effectively, organizations experience revenue leakage (the U.S. healthcare system loses approximately $935 million weekly due to billing and coding errors), increased denials, compliance violations, operational inefficiency, and provider frustration. Organizations with integrated teams see higher clean claim rates, faster collections, lower denial rates, and improved compliance outcomes.
Industry Trends and Market Statistics
Market Size and Growth
The global medical coding market reached USD 38.58 billion in 2024 and is projected to grow to USD 89.49 billion by 2033, expanding at a CAGR of 9.2%. In the U.S. specifically, the medical coding market was valued at USD 21.89 billion in 2024 with expectations to grow at 10% CAGR through 2033.
The medical billing market was estimated at USD 17.76 billion in 2024 and is projected to reach USD 62.65 billion by 2035, exhibiting a CAGR of 12.14%. This robust growth reflects increasing healthcare complexity, regulatory requirements, and the shift toward value-based reimbursement models.
Denial Rate Benchmarks
Denial rates continue climbing across all payer types. Initial claim denials reached 11.8% in 2024, up from 10.2% just a few years earlier. Approximately 41% of providers now face denial rates of at least 10%, according to recent surveys.
By payer type:
- Medicare: 8.4% initial denial rate
- Medicaid: 16.7% initial denial rate
- Commercial payers: 13.9% initial denial rate
- Medicare Advantage: 15.7% initial denial rate
- Managed Medicaid: 15.1% initial denial rate
Denial rates from commercial plans rose by 1.5%, while Medicare Advantage plans saw a 4.8% spike from 2023 to 2024. These increases place significant pressure on revenue cycle operations to improve coding accuracy and billing practices.
Coding Error Statistics
Coding accuracy remains a persistent challenge. CMS reported that the average Part B error rate among all provider types was 10.3% in 2024, with certain specialties experiencing higher rates:
- Internal medicine clinicians: 14.2% error rate
- Family practice clinicians: 11.4% error rate
- Chiropractors: 33.6% error rate
The most commonly billed E/M code, CPT 99214, was also among the most error-prone services. Over $31 billion in improper Medicare payments occurred in 2024, with coding inaccuracies contributing substantially to this figure.
Research indicates that 26.8% of primary diagnosis codes and 9.9% of secondary diagnosis codes contain errors in hospital settings. These inaccuracies affect both reimbursement accuracy and clinical data quality.
Outsourcing Trends
Healthcare providers increasingly turn to outsourcing to address billing and coding challenges. The global medical billing outsourcing market was valued at USD 17.15 billion in 2024 and is expected to reach USD 54.17 billion by 2034, growing at 12% CAGR.
The U.S. medical billing outsourcing market reached USD 6.28 billion in 2024 and is projected to grow at 12% CAGR through 2030. The outsourced segment accounts for approximately 69.69% of medical coding revenue, as providers seek to reduce administrative costs, access specialized expertise, and improve coding accuracy.
Key drivers of outsourcing growth include:
- Shortage of qualified coders and billers in competitive labor markets
- Complexity of coding guidelines requiring specialized knowledge
- Need to reduce operational costs and improve margins
- Desire to focus internal staff on patient care rather than administrative tasks
- Access to advanced technology platforms without capital investment
Automation and AI Adoption
Artificial intelligence is transforming billing and coding operations. AI-powered coding tools can improve accuracy and reduce denials, with practices using AI seeing up to 28% reduction in claim rejections.
In August 2025, Infinx partnered with Maverick AI to introduce instant autonomous medical coding for revenue cycle management. In October 2024, Corti partnered with Tanner Health to accelerate medical coding, reducing administrative workload by 80% and improving billing accuracy.
According to industry data, about 46% of hospitals already use AI-enabled billing services. AI applications now include:
- Automated code assignment from clinical documentation
- Real-time coding suggestions at the point of care
- Predictive analytics for denial prevention
- Natural language processing to extract information from unstructured notes
- Computer-assisted coding that increases productivity by 11-30%
While AI adoption accelerates, the technology complements rather than replaces human expertise. Coders and billers still need to validate AI suggestions, handle complex cases, and ensure compliance with evolving regulations.
Conclusion
Medical billing and medical coding serve distinct yet interconnected functions within revenue cycle management. Coding translates clinical documentation into standardized codes that describe diagnoses and procedures, while billing manages the claim submission and payment collection process.
The key differences lie in their focus, skill requirements, and daily responsibilities. Coders need clinical knowledge and must apply complex coding guidelines accurately. Billers require insurance expertise and must navigate payer requirements to secure timely payment.
Both functions directly impact financial performance. Coding errors trigger claim denials, compliance risks, and revenue leakage. Billing inefficiencies extend accounts receivable days and reduce cash flow. When coding and billing teams work collaboratively within an integrated workflow, organizations achieve better outcomes: higher clean claim rates, faster collections, lower denial rates, and improved compliance.
As denial rates climb to 11.8% and coding complexity increases, accurate billing and coding have never been more critical. Healthcare organizations that invest in skilled professionals, advanced technology, and process integration will maintain financial stability while meeting the demands of an evolving healthcare landscape.
Viaante partners with healthcare organizations to optimize revenue cycle operations through expert medical billing, coding, and compliance support. With deep expertise in healthcare operations, Viaante helps providers improve cash flow, reduce denials, and maintain regulatory compliance while allowing clinical staff to focus on patient care.